Cervical Cancer
Introduction
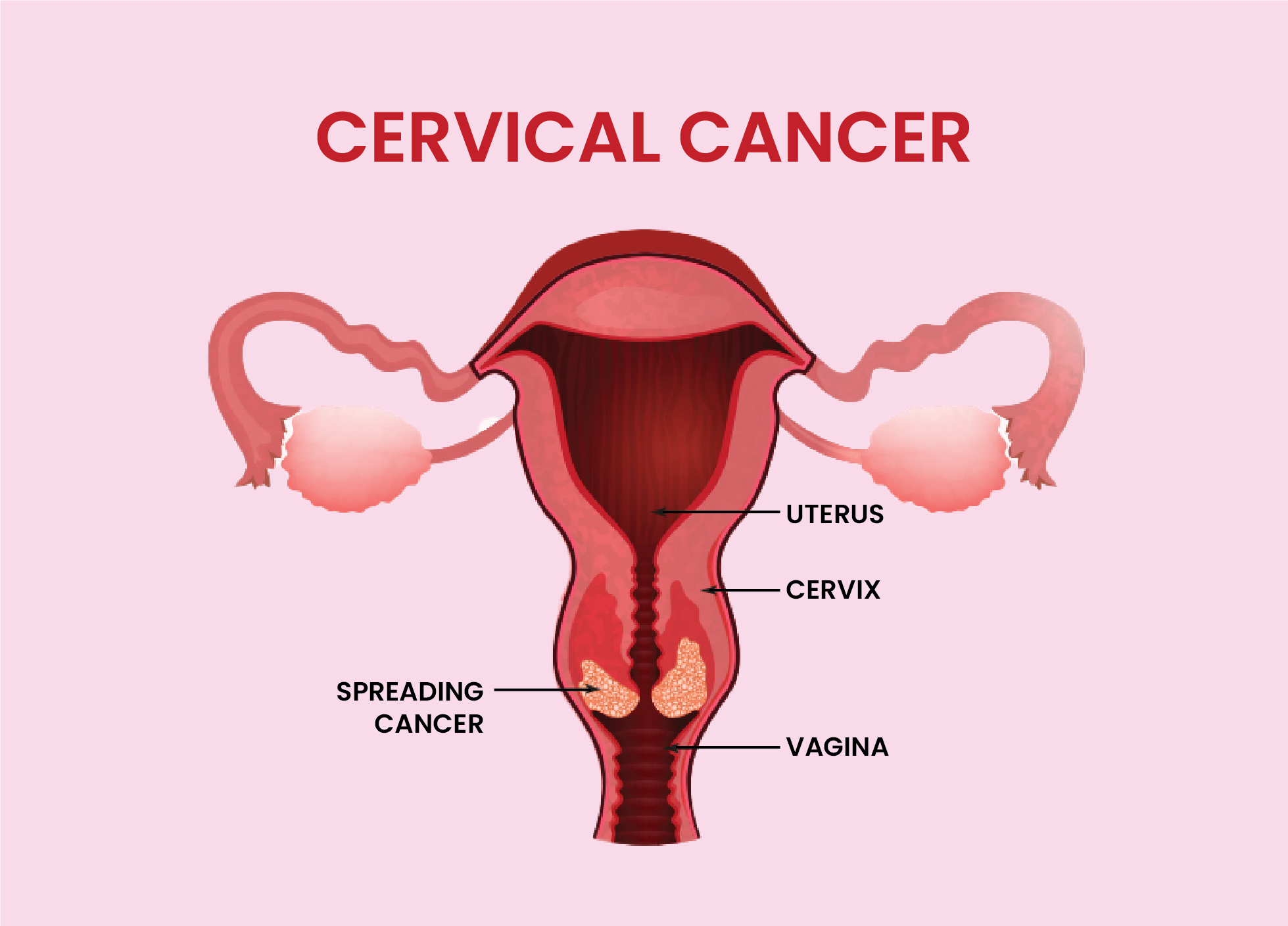
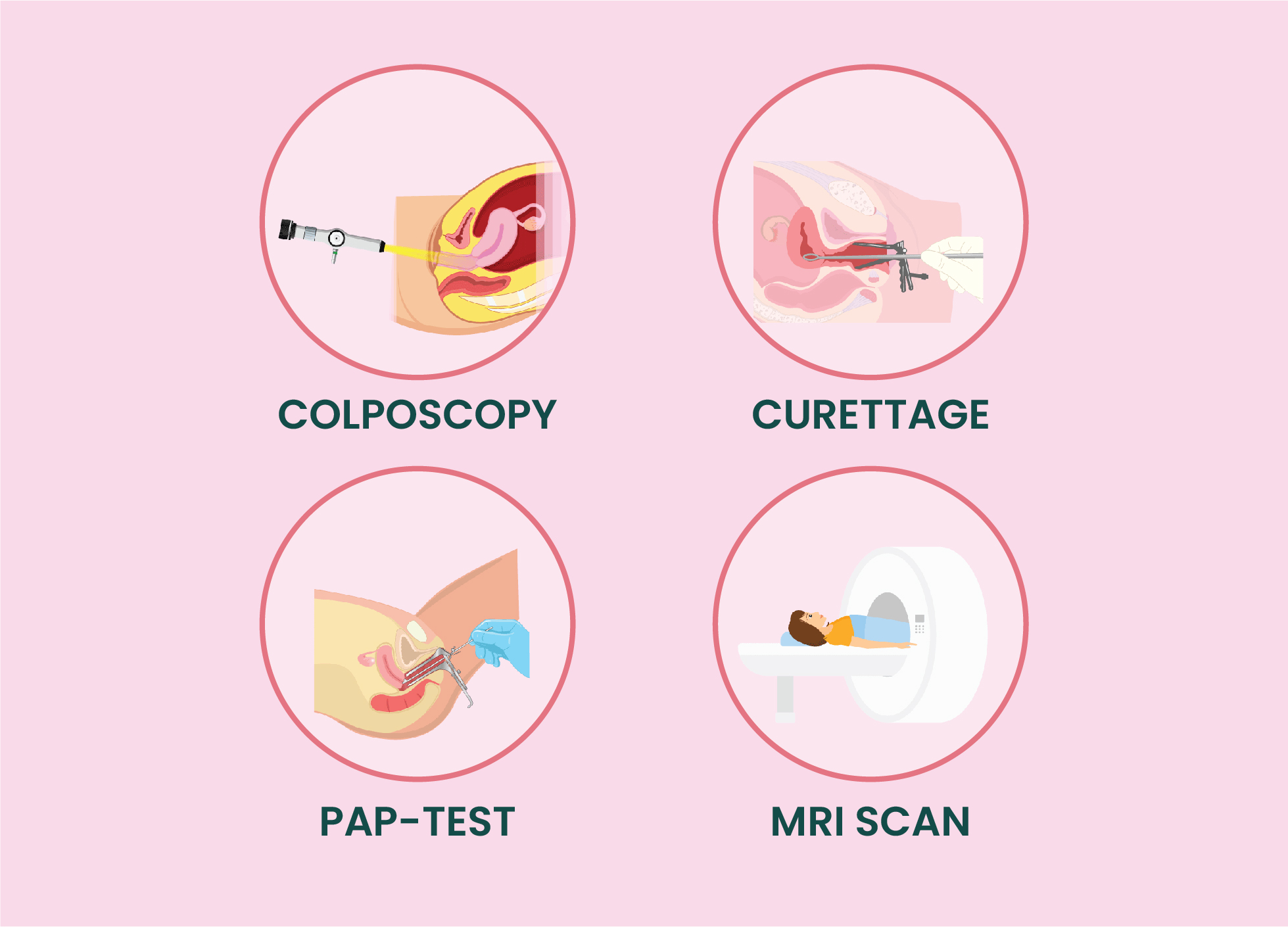
In India, cervical cancer contributes to approximately 6 - 29% of all cancers in women. Cervical cancer occurs in approximately 1 in 53 Indian women during their lifetime compared with 1 in 100 women in more developed regions of the world. Cervical cancer is a condition in which cancer cells appear in the cervix, which connects the uterus to the vagina. Cervical cancer usually takes a long time to develop. During this time, the cells in the cervix convert and grow rapidly. Cervical cancer generally develops very slowly, starting as a pre-cancerous condition called dysplasia. Dysplasia can be detected by a Pap smear. This is why it is so important for women to get regular Pap smears. Undetected, pre-cancerous changes can develop into cervical cancer and spread to the lungs, liver, bladder, and intestines. It can take a long time for pre-cancerous changes into cervical cancer.
TYPES OF CERVICAL CANCER
Cervical cancer is categorized based on the type of cell where it occurs. The most common types of cervical cancer are:
RISK FACTOR
The risk of developing cervical cancer is directly associated with the risk of contracting HPV.
Types
Epithelial ovarian cancer is the most common type of ovarian cancer. Primary peritoneal cancer and fallopian tube cancer are analogous to epithelial ovarian cancer and are treated in the same way. Rare types of ovarian cancer include germ cell tumours, stromal tumours and sarcomas.
Symptoms
In its initial stages, cervical cancer normally does not have symptoms. That is why regular Pap tests are so important, particularly for sexually active women.
Signs and symptoms of cervical cancer include:

Diagnosis
Cervical cancer is one of the most successfully treatable forms of cancer, as long as it is detected early and managed effectively. If cervical cancer is diagnosed inlater stages, it can be controlled with appropriate treatment and palliative care.
Management
Management of cervical cancer depends on the stage, patient co-morbidities, lymph node involvement, and risk factors for recurrence. Treatment may include surgery, Cone biopsy, Trachelectomy, chemotherapy, radiation therapy.

Follow-Up
In patients with higher-risk cervical cancers, clinical follow-up may be performed every 3 months for the first 2 years, every 6 months for years 3 through 5, and then annually.
For patients with low-risk cervical cancer, clinical assessment is less frequent and may be performed every 6 months for the first 2 years, and then annually.
